Introduction
Systemic Lupus Erythematous (SLE), the most prevalent form of lupus, is a chronic autoimmune disease that poses significant challenges in diagnosis and treatment. In SLE, the immune system turns against the body's own tissues, leading to widespread inflammation and tissue damage in various organs. Joints, skin, brain, lungs, kidneys, and blood vessels are among the commonly affected areas, making SLE a complex and multifaceted condition.

Understanding SLE
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disease where the immune system mistakenly attacks the body's own tissues, leading to widespread inflammation and tissue damage.
Diagnosing SLE can be intricate due to its symptoms often resembling those of other illnesses. However, one distinguishing feature of lupus is the butterfly-shaped facial rash that appears across both cheeks, although it may not manifest in all cases. Additionally, certain individuals are predisposed to developing lupus, with triggers ranging from infections and specific medications to sunlight exposure.
Despite the challenges associated with SLE, advancements in medical research and treatment have provided hope for improved management of the disease. By unravelling the complexities of SLE, healthcare professionals can better understand its manifestations and explore effective strategies to address its symptoms and minimise long-term damage.

Types of SLE
There are actually several recognized types of systemic lupus erythematous (SLE), as well as other lupus-related condition
are a few additional types:
- Systemic Lupus Erythematosus (SLE):The most common form of lupus, affecting various organs with symptoms like fatigue, joint pain, skin rashes, and inflammation.
- Discoid Lupus Erythematosus (DLE):Primarily affects the skin, characterized by red, scaly, and raised patches or plaques.
- Drug-Induced Lupus Erythematosus (DILE):Certain medications can cause lupus-like symptoms, which usually resolve after discontinuing the medication.
- Neonatal Lupus:A rare condition in infants born to mothers with lupus autoantibodies, causing skin rash, liver problems, and sometimes heart defects.
- Cutaneous Lupus Erythematosus (CLE):A category including DLE and other forms of lupus that mainly affect the skin. Subtypes include subacute cutaneous lupus erythematous (SCLE) and acute cutaneous lupus erythematous (ACLE). Please remember that it's essential to consult a healthcare professional for an accurate diagnosis and appropriate management if you suspect you have lupus or a related condition.

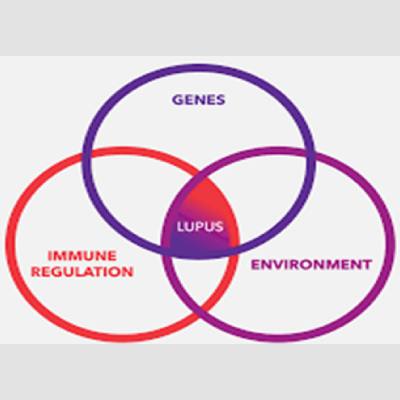
Causes of SLE
Lupus is an autoimmune disease characterised by the immune system mistakenly attacks healthy tissues in the body. The exact cause of lupus is unknown, but it is believed to be a result of a combination of genetic and environmental factors. People with a genetic predisposition to lupus may develop the disease when exposed to certain triggers in the environment. However, the specific triggers are not well understood. Overall, while the cause of lupus in most cases remains unknown, ongoing research aims to better understand the complex interplay between genetics and environmental factors involved in the development of the disease.
Environmental Triggers

Sunlight
Exposure to sunlight can bring on lupus skin lesions or trigger internal responses in susceptible individuals.

Infections
Certain infections can initiate lupus or cause relapses in some people.

Medications
Certain medications like blood pressure medications, anti-seizure medications, and antibiotics can trigger drug-induced lupus. Symptoms usually improve upon discontinuing the medication, but sometimes symptoms persist even after stopping the drug.
Environmental Factors
Triggers may include ultraviolet rays, certain medications, viruses, physical or emotional stress, and trauma.
- Genetics
- Lupus is not linked to a specific gene, but individuals with lupus often have family members with other autoimmune conditions.
- People with an inherited predisposition for lupus may develop the disease when exposed to environmental triggers.
- Sex and Hormones
- Lupus affects women more than men.
- Women may experience more severe symptoms during pregnancy and menstrual periods.
While the cause of lupus in most cases remains unknown it’s important for individuals with lupus or those who suspect they may have lupus to consult with a healthcare professional for an accurate diagnosis and appropriate management. Sanjivani Homoeopathy is a clinic that offers homoeopathic treatments and can provide you with guidance and personalised care based on your specific needs. Seeking professional medical advice is important for proper evaluation and treatment.
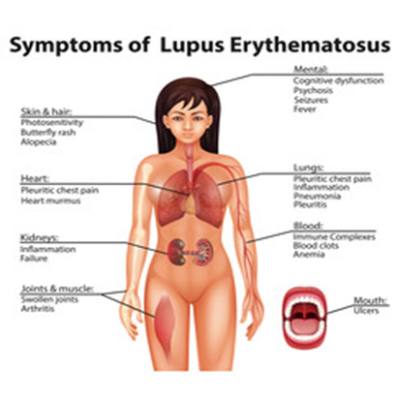
Symptoms of SLE
Symptoms of lupus can vary greatly from person to person, with no two cases being exactly alike. They may appear suddenly or develop gradually, and their intensity can range from mild to severe. These symptoms can also be temporary or persistent. Common signs and symptoms of lupus include:

Fatigue
Feeling extreme tiredness and experiencing low energy

Low-grade Fever
Mild fever resulting from the underlying inflammation, often classified as a fever of unknown origin.

Joint Pain, Stiffness, and Swelling
Pain, stiffness, and swelling in various joints, with frequent involvement of the fingers, wrists, knees, and other joints. Swelling may also occur in the feet, hands legs, and under the eyes
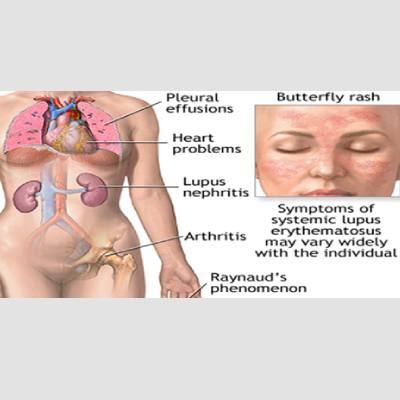
Butterfly-Shaped Facial Rash
A characteristic rash resembling the shape of a butterfly, appearing on the cheeks and bridge of the nose. Rashes may also occur elsewhere on the body.

Shortness of Breath and Chest Pain
Difficulty breathing and chest pain, particularly upon deep inspiration.
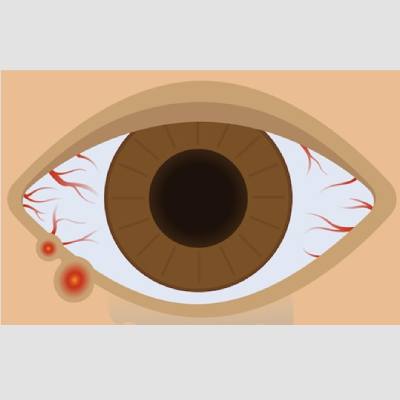
Dry Eyes, Mouth, and Vagina
Persistent dryness in the eyes,mouth, and vaginal area.

Confusion and Memory Loss
Cognitive symptoms such as confusion and memory loss.
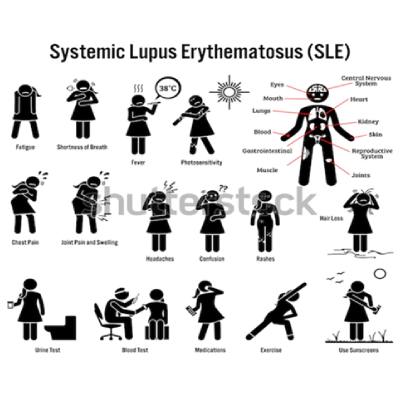
Arthritis
Joint inflammation leading to pain and stiffness.

Depression
Feelings of sadness and hopelessness.

Headaches, Migraines, Seizures, and Stroke
Various neurological symptoms including headaches, migraines, seizures, and, in rare cases, stroke

Hair Loss
Noticeable hair loss or thinning

Pleurisy and Pericarditi
Inflammation of the lining surrounding the lungs (pleurisy) or the heart (pericarditis).
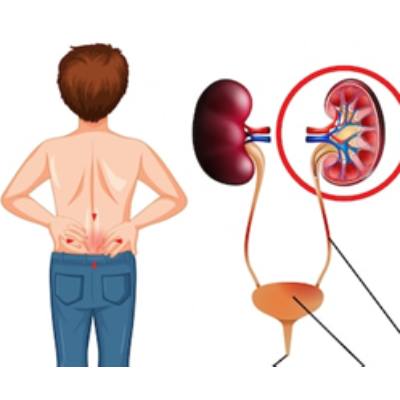
Kidney Problems
Impaired kidney function and associated symptoms.

Nausea, Vomiting, and Abdominal Pain
Gastrointestinal symptoms such as nausea, vomiting, and abdominal pain.

Mouth and Nose Ulcers
Painful ulcers in the mouth and nasal area.

Sensitivity to Sunlight (Photosensitivity)
Increased sensitivity to sunlight, resulting in skin reactions or rashes.
Photosensitivity
Skin lesions that either appear or worsen upon exposure to sunlight.
Raynaud's phenomenon
Fingers and toes turning white or blue in colour when exposed to cold temperatures or during periods of stress.
Anaemia
Low levels of haemoglobin and total blood volume.
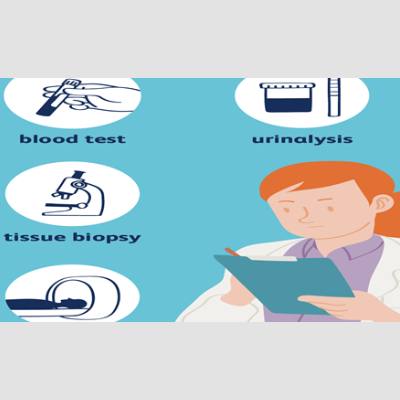
Diagnosis
Diagnosing lupus is challenging due to the considerable variation in signs and symptoms among individuals. The manifestations of lupus can fluctuate over time and share similarities with several other disorders. The diagnosis of lupus is not reliant on a single test but rather on the combination of blood and urine tests, assessment of signs and symptoms, and findings from a physical examination.
Medical history and physical examination:
The doctor will review your medical history and ask about your symptoms, such as fatigue, joint pain, rashes, and other relevant information. They will also conduct a physical examination to look for signs of inflammation, skin abnormalities, and other lupus-related findings
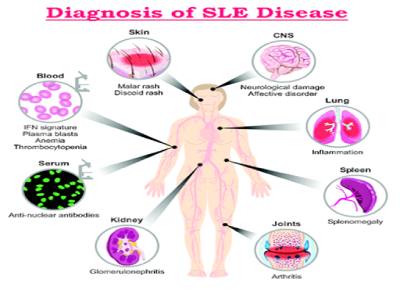
LABORATORY TEST
Blood and Urine Tests may include:
Imaging Test
If doctor suspects that lupus is affecting lungs or heart, he or she may suggest

Chest X-ray
An image of your chest may reveal abnormal shadows that suggest fluid or inflammation in your lungs.

Echocardiogram
This test uses sound waves to produce real-time images of your beating heart. It can check for problems with your valves and other portions of your heart
Complete blood count
This test measures different components of blood, such as red blood cells, white blood cells, and platelets. Lupus can cause abnormalities in these blood cell counts. Complement proteins, such as C3 and C4, may be measured as they can be reduced in lupus.
Erythrocyte sedimentation rate
Erythrocyte Sedimentation Rate (ESR) and C-reactive protein (CRP): These tests indicate the presence of inflammation in the body, which can be elevated in lupus and other conditions.
Assessment of Kidney and Liver Function
Blood tests can evaluate the functioning of your kidneys and liver. Lupus has the potential to affect these organs.
Urinalysis
A urine analysis may be performed to check for the presence of protein or other abnormalities, which can indicate kidney involvement in lupus.
Antinuclear antibody (ANA) test
This test detects the presence of antibodies that target the cell nuclei, which is a common feature in lupus. However, a positive ANA test does not necessarily confirm lupus, as it can also be positive in other autoimmune and non-autoimmune conditions.
(anti-ds DNA)
The anti-double stranded DNA tests- Additional antibody tests may be conducted to detect specific antibodies associated with lupus, such as anti-double-stranded DNA (anti-dsDNA) antibodies, anti-Smith (anti-Sm) antibodies, and antiphospholipid antibodies
Biopsy
Biopsy In certain cases, a small tissue sample (biopsy) from affected organs, such as the skin or kidneys, may be taken for further examination under a microscope. This can help confirm lupus and assess the extent of organ involvement.
Risk Factors
Risk factors for lupus include:

Sex
Lupus is more common in women than men.

Age
Although lupus can affect people of all ages, it is most frequently diagnosed between the ages of 15 and 45.
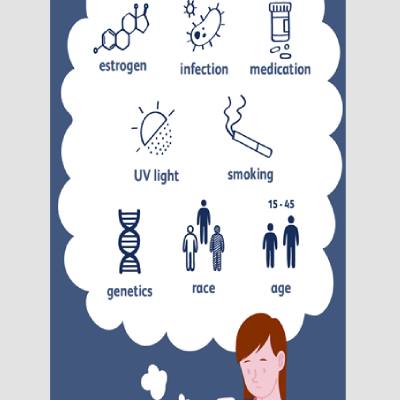
Race
Lupus is more commonly seen in certain racial and ethnic groups, including African-Americans, Hispanics, and Asian-Americans.
Complications
Complications of lupus include:
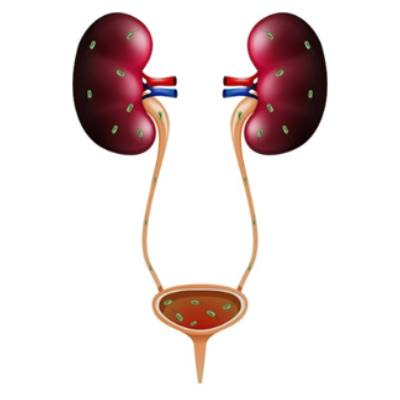
Kidneys
Lupus can cause serious kidney damage, leading to kidney failure, which is a leading cause of death among people with lupus.

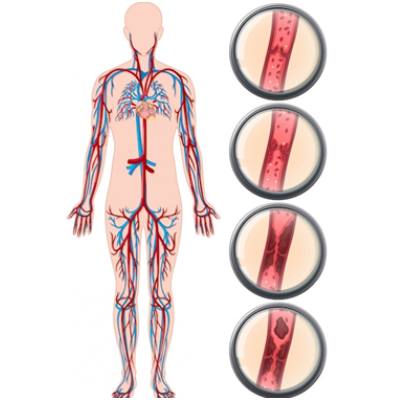
Blood and Blood Vessel Problems
Lupus can cause blood-related issues like anaemia, increased risk of bleeding or blood clotting, and inflammation of blood vessels (vasculitis).
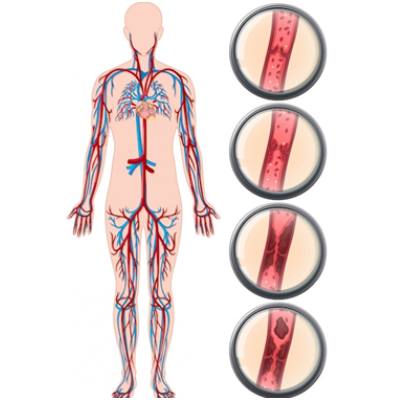
Heart Involvement
Lupus can lead to inflammation of the heart muscle, arteries, or the membrane around the heart (pericarditis). It also increases the risk of cardiovascular disease and heart attacks.
Brain and Central Nervous System Involvement
Lupus can affect the brain and central nervous system, leading to symptoms such as headaches, dizziness, behaviour changes, vision problems, strokes, seizures, and memory difficulties.
Lung Involvement
Lupus increases the risk of inflammation of the lining of the chest cavity (pleurisy) and other lung complications.
Other types of complications
Pregnancy Complications
Women with lupus have an increased risk of miscarriage and high blood pressure during pregnancy. It's important to note that complications can vary among individuals, and proper medical management and regular healthcare follow-ups are essential in reducing the risk and managing any complications that may arise. If you have concerns about complications associated with lupus, it is recommended to consult with a healthcare professional for personalised advice and guidance.
Bone Tissue Death (Avascular Necrosis)
Lupus can diminish the blood supply to a bone, leading to bone damage and collapse.
Infections
People with lupus have a higher vulnerability to infections due to the disease and its treatments weakening the immune system.
Cancer
Although the risk is small, having lupus appears to increase the overall risk of developing certain types of cancer.
Homoeopathy and SLE
Homoeopathy offers a holistic approach to managing Systemic Lupus Erythematosus (SLE), focusing on individualised care that addresses both physical and emotional symptoms. This medicine are made from natural substances in highly diluted forms to stimulate the body's self-healing processes.
Homoeopathic Remedies for SLE- Systemic Lupus Erythematous
- Rhus Toxicodendron
- Effective for joint pains, stiffness, and swelling in SLE.
- Reduces joint pains and stiffness that worsen during rest and improve with motion.
- Warm applications and joint massage provide relief.
- Acts on both skin and joints in cases of lupus.
- Arsenic Album
- Helps manage fatigue in SLE.
- Individuals feel exhausted with minimal exertion.
- Desire to lie down all the time.
- Anxiety and restlessness accompany fatigue.
- Natrum Mur
- Used to treat sun-induced skin lesions in SLE.
- Symptoms include skin rash or vesicular eruption from sun exposure.
- Itching, stinging sensation, and crawling sensation on the skin may be present.
- Belladonna
- Effective for SLE-related headaches.
- Most people experience congestive and throbbing headaches.
- Extreme fullness in the head.
- Headaches worsen with noise and light, but pressure on the head provides relief.
- Mercurius Solubilis
- Well-suited for oral and/or nasal-pharyngeal ulceration in lupus.
- Borax
- Best suited for mucosal ulceration, particularly in the oral mucosa.
- Syphilinum
- Can be given as an intercurrent dose for cases with syphilitic miasma in the background.
- Useful for painless red malar rash or butterfly rash with thickening and exfoliation.
- Suited for ulcerations of oral and nasopharyngeal mucosa.
- Ferrum Phosphoricum
- Given in cases with febrile conditions, malaise, fatigue, hair loss, and anaemia due to lupus or its medications.
- Can be used in low potencies in biochemical form alongside other medicines.
- Ferrum Metallicum
- Suitable for acute lupus erythematous with red acute rash and oral mucosa involvement.
- Also useful in later chronic stages with signs of anaemia of chronic disease or hemolytic anaemia.
- Aconite
- Natural treatment for managing dry eyes in SLE.
- Symptoms include dryness, heat, and sand-like sensation, sensitivity to light (especially sunlight), itching, lachrymation, and burning in the eyes.
- Ipecac
- Well-indicated for treating depression in SLE.
- Key features include extreme sadness with excessive weeping.
- Desire to be alone is present along with the above features.
- Colocynthis
- Prepared from the pulp of the fruit of the plant Citrullus Colocynthis or Bitter Apple.
- Effective for relieving abdominal pain in SLE.
- Pain worsens after consuming even the slightest food or drinks.
- Bending over double or pressing the abdomen helps relieve the pain.
- Phosphorus
- Effective for managing hair loss in SLE.
- People experience excessive hair fall, often in bunches.
- Hair fall may occur in circumscribed spots.
- Copious dandruff may be present along with hair fall.
Benefits of Homoeopathic Treatment
- Individualised Care: Homoeopathy recognizes that each person is unique. A homoeopath will assess your symptoms, medical history, and lifestyle to prescribe a personalised treatment plan tailored to your needs.
- Gentle and Natural: Homoeopathic remedies are derived from natural substances and are known for their minimal side effects. They work in harmony with the body, promoting self-healing and overall well-being.
- Holistic Approach: Homoeopathy takes into account not only the physical symptoms but also the emotional and mental aspects of an individual. It aims to restore balance at all levels, providing comprehensive care.
- Long-Term Relief: By addressing the underlying causes of Ulcerative Colitis,homoeopathy strives to achieve long-term relief and improved quality of life.
Consulting a Homeopath
To achieve the best results with homoeopathic treatment for SLE, it is essential to consult a qualified Sanjivani homoeopathic physician. A detailed case history and thorough symptom analysis are crucial for selecting the most appropriate remedies. A professional Sanjivani homoeopath can provide a personalised treatment plan, ensuring effective symptom management and improved quality of life.
Sanjivani Homeopathy Clinic USP
- No homoeopathy Dietary Restrictions:
Allows patients to enjoy foods like onion, garlic, and coffee, ensuring a stress-free treatment journey.
- 24/7 Online Consultations:
Enables convenient access to doctors with detailed counseling, history management, and follow-ups.
- Highly Skilled Team:
Experienced BHMS and MD doctors, supported by multilingual and professional staff.
- Patient-Centric Care:
Simplifies treatment with modern, adaptable solutions and clear communication.
Click Here for Detailed "Sanjivani USP"
FAQ's
- What is homoeopathy ?
Homoeopathy is a holistic science which belives in the law of Similia Similibus Curenter i.e Like Cures Like .It was discovered by Dr Samuel Christian Hahnemannn in 1796.
- Is there any side effects of homoeopathy?
As homoeopathic medicines are made from natural substances this medicines have no side effects and are completely safe to consume
- Is there any diet restriction to take homoeopathic medicines?
There are no diet restrictions for homoeopathic medicines. One should only avoid eating or drinking any liquid other than water at least 30 minutes before and after taking homoeopathic medicines.
Click Here for "Frequently Asked Questions."
Conclusion
Homoeopathic medicines offer a valuable supportive role in the management of Multiple Sclerosis.. Treatment is individualised, making it essential to consult with a qualified Sanjivani homoeopathic physician to develop an appropriate and effective treatment strategy.
Disclaimer :The information provided in this blog is for educational purposes only and should not be considered medical advice. Please consult with a qualified healthcare professional before starting any treatment for SLE or any other medical condition.


